U.S. President Joe Biden tested positive for COVID-19 a third time on Thursday after taking an antiviral drug treatment, but an infectious disease expert says “rebound” cases are not an unheard phenomenon and can happen even in people who don’t get the Paxlovid treatment.
“We’re hearing about post-COVID rebound primarily because that’s what happened to President Joe Biden, who got treated (with Paxlovid) and perhaps other treatments…And what we know is that COVID rebound isn’t an unheard of phenomenon,” Donald Vinh, an infectious diseases specialist at McGill University Health Centre, told Global News.
Such cases have been reported before, he said.
“There are rebound cases that occur in people who are also not treated (with Paxlovid),” he added.
According to the Centers for Disease Control and Prevention (CDC), COVID-19 rebound is characterized by a recurrence of symptoms or a new positive viral test after having tested negative.
“There is no standardized definition for what COVID-19 rebound means…but now it’s believed you’d have both a symptom rebound and a positive viral test to have a post-COVID rebound,” said Vinh.
Should masking be reinstated? The latest COVID-19 update and more
Biden, 79, had emerged from isolation on Wednesday last week after testing positive for COVID for the first time on July 21. He tested positive again on Saturday in what the president’s physician described as a “rebound” case seen in a small percentage of patients who take the antiviral drug Paxlovid.
White House COVID-19 coordinator Dr. Ashish Jha told reporters on Monday that data “suggests that between 5 and 8 percent of people have rebound” after Paxlovid treatment.
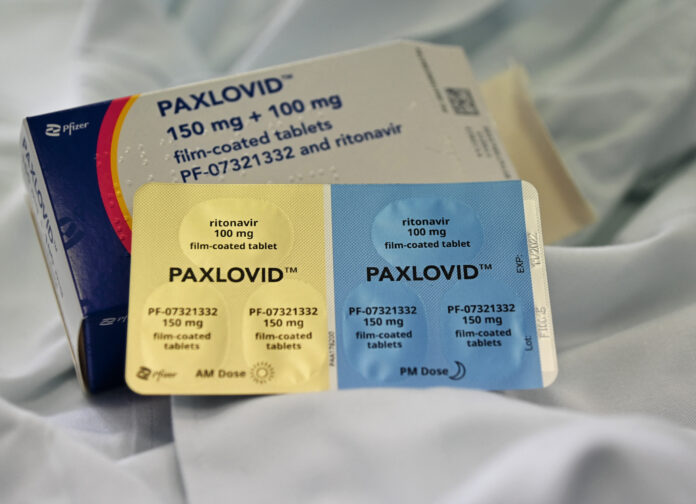
Dozens of individuals have reported rebounding COVID symptoms on social media or to the U.S. Food and Drug Administration after taking Paxlovid, but Pfizer suggested in May that the experience is rare.
Pfizer’s Paxlovid treatment helps prevent hospitalization and death due to COVID-19. It is recommended for early stage treatment of mild to moderate COVID-19 among persons at high risk for progression to severe disease, said the CDC in a health advisory.
Pfizer has said that from the more than 300,000 patients it is monitoring who received the five-day treatment, around one in 3,000, or about 0.03 per cent, reported a relapse after taking the pills.
In a June 2022 study published in the Journal of Infection, researchers found that “it is unclear if COVID-19 rebound associated with anti-viral drug treatment is a distinct clinical phenomenon” and suggested that the failure to respond to the therapy may be an explanation.
“We have to understand that this doesn’t reflect a failure of Paxlovid because what we have to do is compare that to what would happen in the absence of treatment,” said Vinh. He added that without treatment people who are at risk would be more prone to severe illness and even death.
He also said that this is not unique to COVID and a rebound of symptoms can take place from a variety of viral infections.
Trending Stories
Researcher says Canada’s ‘largest documented hailstone’ fell Monday in Alberta
Earth is spinning faster than normal, and we just had our shortest day in recent history
Doctors call for better access to COVID-19 treatment drug Paxlovid – Apr 13, 2022
Vinh said people with COVID-19 rebound can be contagious depending on whether they have a recurrence of symptoms only or a viral rebound.
He explained that a recurrence of symptoms may reflect that the person’s immune system is trying to fight off whatever remains of the virus it finds that’s causing the symptoms.
“On the other hand, if you have a viral rebound with or without symptoms, it’s very possible that you can be contagious to other people,” said Vinh.
Vinh said having COVID-19 rebound doesn’t mean that the risk of getting severe disease is higher.
A study published last month in the Oxford Academic journal found that in a cohort of 483 high-risk patients treated with Paxlovid in 2019, two patients (0.4 per cent) required hospitalization by day 30. Four patients (0.8 per cent) experienced a rebound of symptoms, which were generally mild, at a median of nine days after treatment, and all resolved without additional COVID-19-directed therapy.
“It doesn’t seem to be a major severe phenomenon from a hospitalization perspective,” said Vinh. But can it “lead to ongoing community transmission? That’s something where the data is not there yet,” he said.
Lack of public data leads to pause of innovative COVID-19 project
Vinh said the studies he has seen so far on rebound COVID-19 mostly involved people who were not vaccinated.
“We use Paxlovid in people who have a high risk of developing severe cases of complicated COVID, so those people are also strongly encouraged to be multi-vaccinated,” he said.
He said it remains to be seen whether the combination of being vaccinated and taking the treatment can further reduce the risk of rebound.
“I want to emphasize that…rebound COVID-19 doesn’t mean we forgo treatment and it doesn’t mean we forgo vaccines,” said Vinh.
He said that vaccination protects people against severe illness from COVID and that’s a huge part of why it’s encouraged.
“That same logic extends to treatments. If you are recommended to get treatment, that means you’re considered, medically speaking, to be at high risk for either severe or complicated disease,” Vinh said.
He said rebound COVID happens “very infrequently” and the benefits of treatments and vaccines outweigh the risks.
“A rebound phenomenon should not dissuade people from getting what they need,” said Vinh.
There have been multiple reports of possible reinfection with COVID-19 in Canada, “however, supporting evidence is often insufficient to allow confirmation,” the Public Health Agency of Canada states on their website.
The agency said that reported episodes of reinfection “range from less than two to 4.5 months.”
However, “transmission from an individual(s) who have been reinfected to another has not been demonstrated,” PHAC said on their website. “But the data is very limited and may change.”
Back to school prep: Getting your child mentally prepared to go back to class
PHAC recommends that if a person gets re-infected then it’s important that they maintain physical distancing and wear a mask.
“PCR positivity may persist or fluctuate for weeks or in some cases months, and positive results, particularly within three months of a previous infection, may not represent a true reinfection,” said the agency.
“However, it is not clear how soon after a COVID-19 diagnosis reinfection may occur and it has been reported within less than two months,” it added.
— with files from Reuters and The Associated Press
© 2022 Global News, a division of Corus Entertainment Inc.